Leprosy – Clinical Aspects
Leprosy, also called Hansen’s disease, is a chronic disease caused by a bacillus, Mycobacterium leprae. M. leprae multiplies slowly and the incubation period of the disease, on average, is five years. In some cases, symptoms may occur within one year but can also take as long as 20 years to occur. The disease mainly affects the skin, the peripheral nerves, mucosa of the upper respiratory tract, and also the eyes. Leprosy is curable with multidrug therapy (MDT).
Transmission of leprosy
Experts believe leprosy is transmitted mainly through the moisture expelled from the upper respiratory tract of an untreated leprosy patient, through sneezing or coughing (droplet infection). Leprosy does not spread by skin contact. However, those who live in close contact with an untreated patient for a long time, especially in cramped and confined spaces, can be infected. A patient does not spread the disease after starting treatment. All individuals infected with the bacteria do not develop leprosy, as 95% of the population has natural immunity to the disease. Leprosy is not hereditary and it is not spread by touch as the bacteria are incapable of crossing intact skin.
Signs and symptoms of leprosy
The first sign of leprosy is usually the appearance of light patches on the skin accompanied by a reduction or loss of sensation over the patches. Peripheral nerves (nerves in the limbs and head, outside the central nervous system) also can get affected in leprosy. Nerve involvement can result in weakness, numbness and paralysis of hands and feet. If neglected, this nerve damage can progress to deformities, like claw hands, foot drop and paralysis of eyelids. Injuries to anaesthetic limbs and eyes can result in ulcers, loss of toes/fingers and limbs, and blindness.
Classification of leprosy
Leprosy has been classified as Paucibacillary (PB) or Multibacillary (MB) types of leprosy, based on the number of skin lesions, nerve involvement and bacteriological status. Correct classification helps in selecting the right treatment regimen for the patient.
| Characteristic | PB (Paucibacillary) | MB (Multibacillary) |
|---|---|---|
| Skin lesions | 1 – 5 lesions | 6 and above |
| Peripheral nerve involvement | No nerve or only 1 nerve +/- 1 to 5 lesions | 1 nerve irrespective of number of skin lesions |
| Skin smear for leprosy bacteria | Negative at all sites | Positive at any site |
Note: If skin smear is positive, irrespective of the number of skin and nerve lesions, the disease is classified as MB leprosy, but if skin smear is negative, it is classified on the basis of the number of skin and nerve lesions.
Treatment
Until the late 1940s, physicians all over the world treated leprosy patients by injecting them with oil from the chaulmoogra nut, a treatment recommended in Sushruta Samhita, an ancient Sanskrit text on medicine and surgery (circa 600 BC).
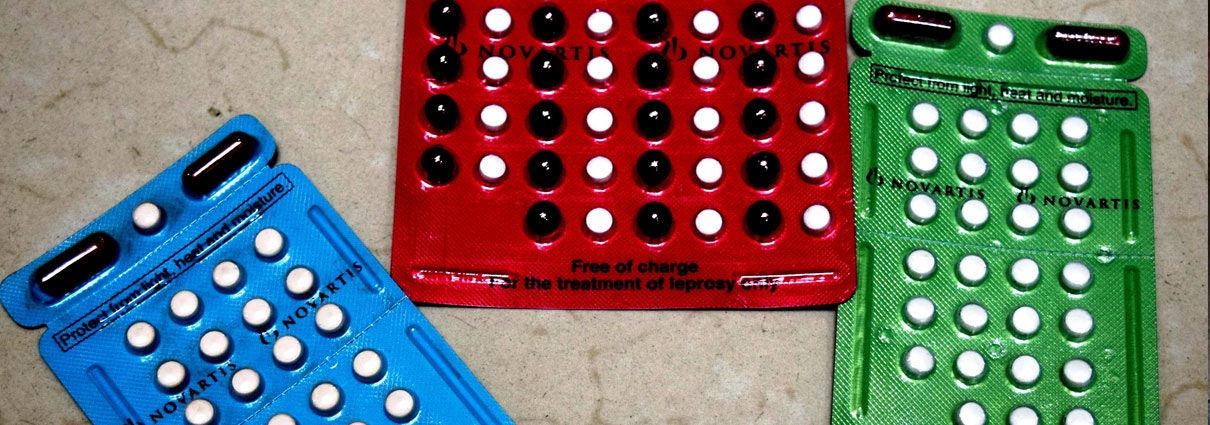
The first breakthrough came in the 1940s with the discovery of the drug, dapsone. The duration of dapsone treatment was for many years, and in some cases, for the entire lifetime. Then M. Leprae began to develop resistance to dapsone, and in the early 1960s, rifampicin and clofazimine were found to be effective. These were added to dapsone to make the treatment regimen more effective. That is how multidrug therapy (MDT) for the treatment of leprosy came into being. In 1984, the World Health Organization (WHO) recommended MDT as a cure for leprosy. MDT takes six months to a year to cure leprosy completely. After the first dose of this medication, patients are no longer infectious, and they do not transmit the disease to others. Since 1995, the WHO has been distributing MDT in convenient monthly calendar blister packs, free of cost. The drugs are manufactured free of cost for the WHO by Novartis.
Once detected and treated by MDT, in 98% of the cases, leprosy ceases to be contagious. Early diagnosis and proper treatment are crucial in stopping transmission and preventing disability.
Watch our video, Taking MDT simplified, to know more about MDT.
Potential complications of leprosy
Complications of leprosy occur mostly if the disease is not diagnosed early and treated effectively. Some of the complications that can occur due to delayed diagnosis and treatment are irreversible loss of sensation (usually begins in extremities), permanent nerve damage (usually in extremities), muscle weakness and progressive disfigurement of toes, feet, fingers, nose, etc. Sensory loss can lead to people injuring body parts without being aware of it. This can lead to ulcers and infection.
Two types of deformities
Deformities due to leprosy are graded into:
- Grade 1 deformity (impaired sensation, no visible impairments, etc)
- Grade 2 deformity (visible deformity)
Reactions in leprosy (lepra reaction)
Lepra reactions are the body’s immune system responding to leprosy-causing bacteria. It is important to manage reactions as they are sometimes severe and result in new nerve damage. This can lead to disabilities, such as loss of sensation and deformities of hands, feet and eyes. There are two types of reaction.
Type 1 reaction
Type 1 reaction is characterised by the development of redness and swelling of the existing patches. When the reaction occurs in nerves, there is a loss of function and pain. Left untreated, it can cause permanent loss of nerve function resulting in peripheral sensory (anaesthesia) and/or motor nerve damage (muscular paralysis).
Type 2 reaction (Erythema Nodosum Leprosum)
As against Type I reaction, Type 2 reaction occurs more often in patients with a heavy load of bacteria. It is characterised by painful and tender red nodules on the skin. This is accompanied by fever, joint pain, painful eye complications and involvement of internal organs (like, lymph nodes, liver, kidneys and testes).
Self-care in leprosy
Leprosy is curable, but the nerve damage resulting from leprosy, if detected late, is irreversible. Loss of sensation (due to nerve damage) leaves hands, feet and eyes susceptible to injury and this can lead to infection and disabilities. Persons affected by leprosy with nerve function impairment, need to practise self-care to avoid such complications.
They should be taught to care for their hands and feet by soaking them in water, scraping away dead skin, and moisturising (soaking, scrubbing, oiling). They should also be taught to examine their hands and feet for sores and ulcers. Protecting anaesthetic hands and feet and eyes is important, and they should be taught how to protect their hands while working in the field or in the kitchen by using gloves or wrapping some soft material around the handles of tools. They should be advised to wear protective footwear with soft insoles (like, microcellular rubber) to protect their feet and to use protective glasses to protect their eyes when they are out in the sun or performing tasks that pose injury risks to eyes.
Reconstructive surgery
These are surgical procedures to correct deformities and restore the function of hands, feet, eyes, and cosmetic procedures to correct disfigurement of the face that occurs due to leprosy. Reconstructive surgery helps in improving function, restoring appearance, increasing self-confidence and self-esteem. Deformities perpetuate stigma and discrimination – hence corrective surgery is very important in addressing stigma related to leprosy. The late Dr Paul Brand pioneered these surgeries.
Current leprosy situation
Multidrug therapy (MDT) was introduced as a safe and effective cure for leprosy in 1982, and since then there is a significant change in the global leprosy situation – the prevalence of the disease reduced from over 5 million cases in the mid-1980s to a little over 200,000 at the end of 2018.
Data published by the World Health Organization (WHO)
show that in 2019, a total of 202,185 new cases of leprosy were reported from 160 countries. India was at the top of the list with 114,451 cases (56.61 per cent of the total caseload), followed by Brazil (27,863 cases, that is 13.78 per cent of the caseload) and Indonesia (17,439 new cases, that is 8.63 per cent of the caseload). Together, these three countries accounted for 79.01 per cent of the global caseload.
Globally, every two minutes someone is diagnosed with leprosy, and in India, every four minutes someone is diagnosed with leprosy!
What is the overall outlook?
The overall outlook is good if the disease is diagnosed early and treated effectively. Early treatment prevents serious health complications and stops the spread of the disease.
Important points to remember:
- Leprosy is caused by a bacterium, and is not a curse of God; it is not the result of past sins.
- Leprosy is like any other disease. It is one of the least infectious diseases; it is less contagious than common cold or influenza.
- A skin patch that is raised or flat, light or less pigmented than the surrounding skin with decreased sensation (touch, pain and heat), and/or muscle weakness or paralysis (especially in the eyelids, hands and feet) may be leprosy. It is important to see a health worker or a medical professional as soon as one notices any of these skin changes.
- Leprosy is not hereditary. Children born to persons with leprosy/cured of leprosy do not have leprosy at the time of birth.
- Leprosy is curable with multidrug therapy (MDT), a combination of three antibiotics – rifampicin, clofazimine and dapsone. MDT takes six months to a year to cure leprosy.
- MDT stops transmission to other individuals.
- Medical treatment for leprosy is available free of cost in all government hospitals and leprosy hospitals run by NGOs.
- Early detection and appropriate treatment prevent deformities and disabilities.
- There is no need to isolate leprosy patients. Casual touch, like shaking hands, playing, eating or travelling together, working in the same office will not transmit or spread leprosy.
- People affected by leprosy have the same rights as anyone else. Respect their rights. Do not discriminate against them.